Team profile by Sarah Arthur, Rebecca Shelby, Annika Agrawal, Annabelle Feibel, Michelle Huang, Shernice Martin, Kayle Park, Meghan Quinlan and Danica Schwartz
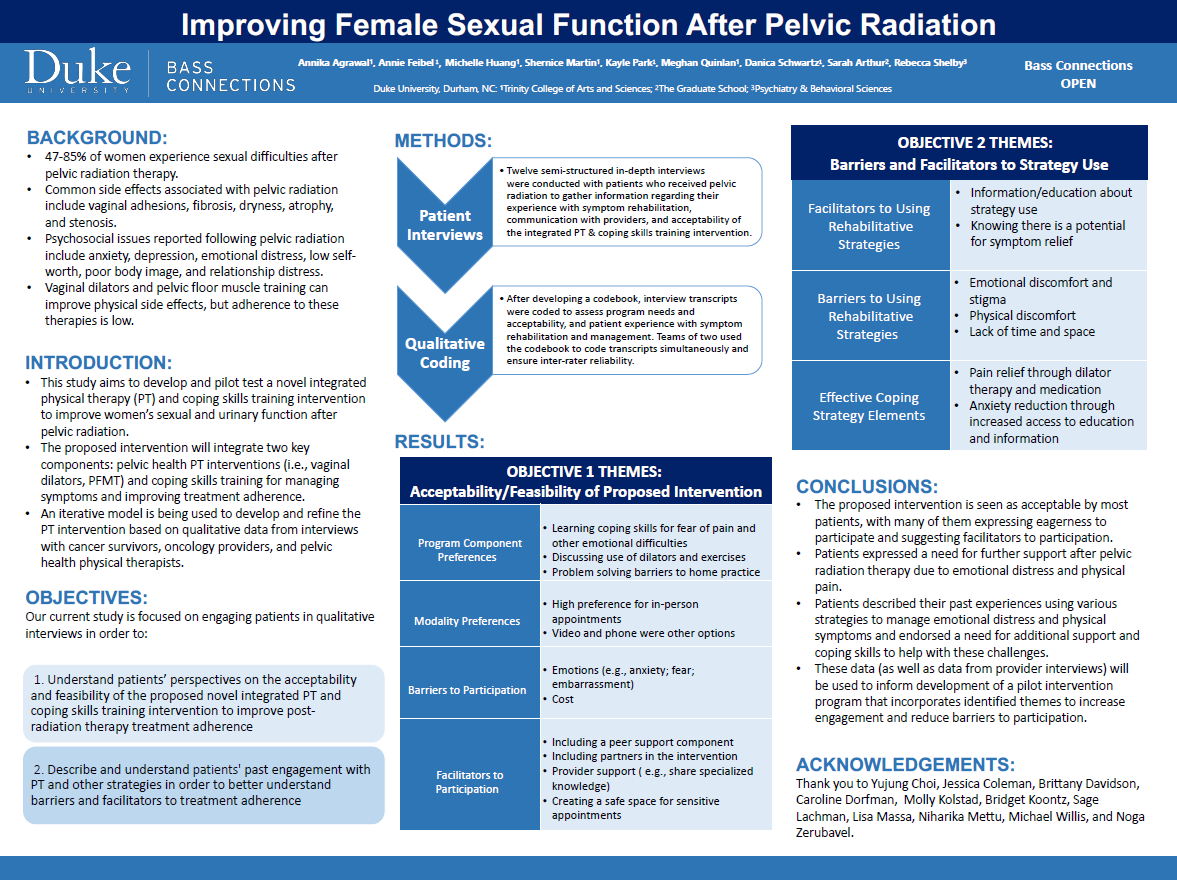
In 2020, more than 156,000 new cases of gynecologic, bladder, rectal and anal cancers were diagnosed among female patients in the United States. While survivorship is high, patients frequently experience devastating and long-lasting side effects of treatment. Among patients who undergo pelvic radiation, 47-85% experience difficult side effects such as vaginal adhesions, fibrosis, dryness, atrophy and stenosis.
Few treatments exist to help women manage pain, improve sexual function and cope with genito-pelvic changes. While vaginal dilators and pelvic floor muscle training are commonly recommended by oncology care providers, adherence to these therapies is low. One novel approach to improving adherence and engagement in recommended treatments is to develop interventions grounded in the biopsychosocial model of pain, which is based on research that highlights the associations between emotional distress, cognitions and pain processing.
With members from Duke Cancer Institute (DCI), Duke Cancer Symptom Management and Support, Duke Women’s Health Physical Therapy and Duke Psychiatry & Behavioral Sciences, this team collaborated to complete the initial stages of intervention development for an integrated pelvic floor physical therapy and coping skills program designed to improve sexual function among women treated with pelvic radiation.
The team interviewed patients with gynecologic, bladder, rectal and anal cancers in order to better understand patient needs and facilitators and barriers to treatment engagement. Further, the team used a qualitative description approach to code and analyze data gathered from interviews.
Key themes suggested that patients view the integrated pelvic floor physical therapy program as necessary and acceptable. Additionally, data suggested that such a program will need to address common difficulties, such as fear of pain and other emotional difficulties (e.g., shame related to genital self-image). Patients also provided a number of suggestions to facilitate participation and engagement in the program, such as including partners in the intervention (as appropriate), and finding ways to create a safe space for these sensitive appointments.
These data, as well as data from provider focus group interviews, will be used to inform the development of the study protocol and patient materials for a pilot intervention planned for fall 2023.
Improving Female Sexual Function After Pelvic Radiation
Poster by Annika Agrawal, Annabelle Feibel, Michelle Huang, Shernice Martin, Kayle Park, Meghan Quinlan, Danica Schwartz, Sarah Arthur and Rebecca Shelby