Improving Health Communication for All Patients
Project Team
Launched in 2017, REGAIN is a collaboration between Duke Health (including the School of Medicine and the School of Nursing) and Duke University. The overarching aim of REGAIN is to implement a roadmap for goals of care conversations for Duke Health patients who have serious illnesses. Led by the Duke Center for Palliative Care and supported by the health system and academic partners, REGAIN is Duke Health’s strategy for ensuring that all patients have access to open, accurate and empathetic communication about their goals for care.
The project team wrestled with a series of conceptual and strategic questions meant to guide Duke Health’s efforts to improve communication for all patients, such as:
- What does good communication look like?
- Where are the needs for communication greatest?
- What are the barriers to communication in a busy clinical setting?
- Can advances in communication improve health-related outcomes such as quality of life, healthcare utilization and survival?
Team members pursued individual projects that yielded new datasets, papers for publication and preliminary data and analysis for a grant proposal.
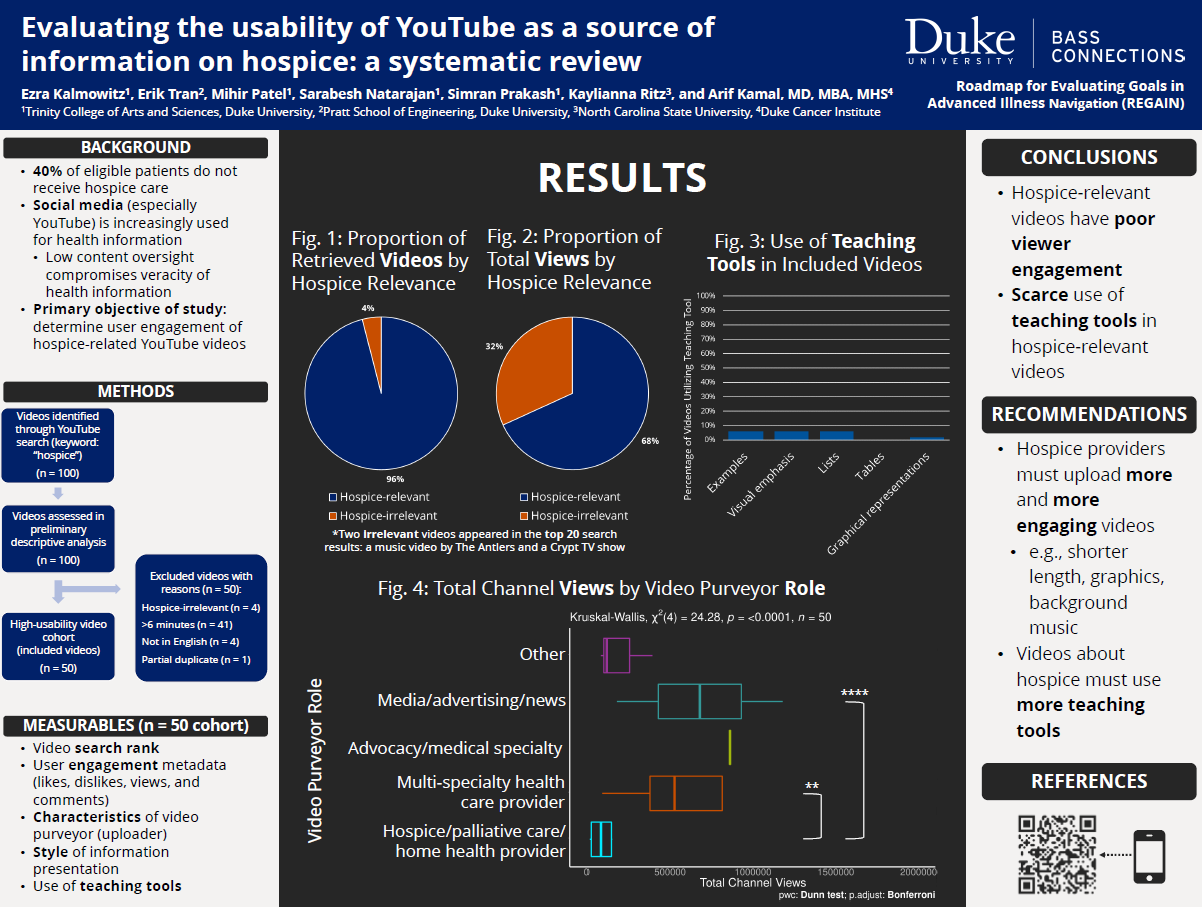
Evaluating the Usability of YouTube as a Source of Information on Hospice: A Systematic Review
Poster by Ezra Kalmowitz, Erik Tran, Mihir Patel, Sarabesh Natarajan, Simran Prakash, Kaylianna Ritz and Arif Kamal
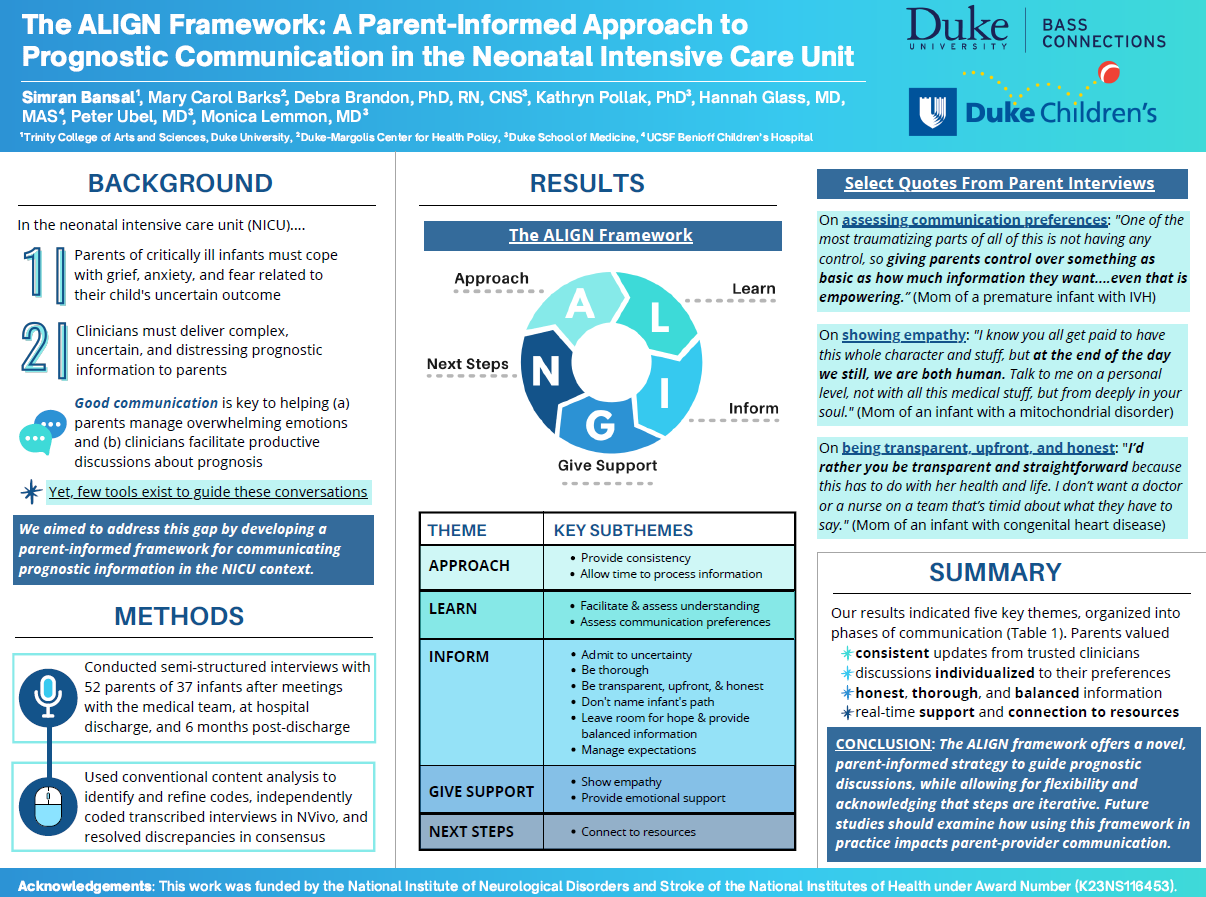
The Align Framework: A Parent-informed Approach to Prognostic Communication in the Neonatal Intensive Care Unit
Poster by Simran Bansal, Mary Carol Barks, Debra Brandon, Kathryn Pollak, Hannah Glass, Peter Ubel and Monica Lemmon
Clinicians often communicate complex, uncertain and distressing information about neurologic prognosis to parents of critically ill infants. And yet, few tools exist to guide prognostic communication. Through semi-structured interviews with parents in the neonatal intensive care unit, we developed the ALIGN framework, a five-phase parent-informed strategy to help clinicians effectively communicate neurologic prognosis.
Meeting of the Minds: Discussion of Brain Imaging for Critically Ill Infants
Poster by Madison Canfora, Mary C. Barks, Margaret H. Bost, Sarah Bernstein and Monica E. Lemmon
My individual inquiry fits into the REGAIN team's broader theme of outreach development to advocate for open and empathetic communication to achieve patient-directed goals.
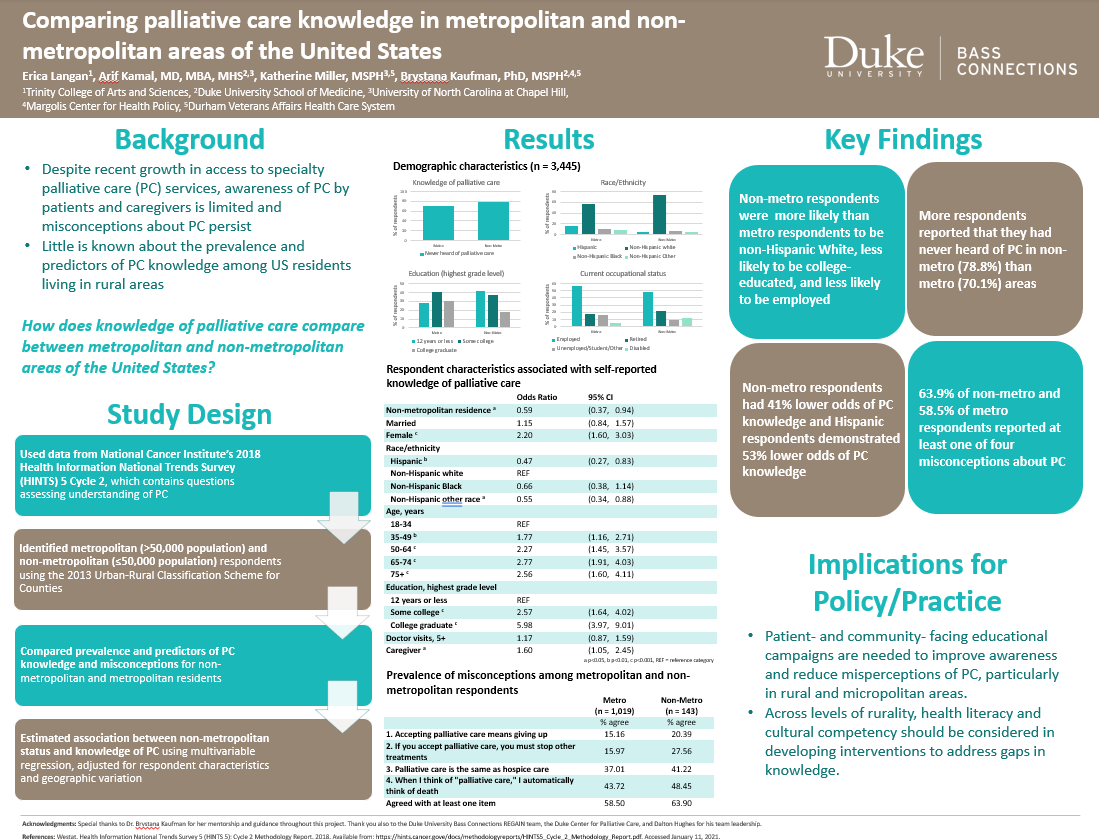
Comparing Palliative Care Knowledge in Metropolitan and Non-metropolitan Areas of the United States
Poster by Erica Langan, Arif Kamal, Katherine Miller and Brystana Kaufman
Despite recent growth in access to specialty palliative care (PC) services, awareness of PC by patients and caregivers is limited and misconceptions about PC persist. Using data from the National Cancer Institute (NCI)’s 2018 Health Information National Trends Survey (HINTS) 5 Cycle 2, which contains five questions assessing understanding of PC, we compared prevalence and predictors of PC knowledge and misconceptions for non-metropolitan and metropolitan respondents. We found that, controlling for other factors, non-metro residence was associated with a 41% lower odds of PC knowledge (odds ratio [OR] = 0.59; 95% confidence interval [CI] = 0.37, 0.94; p < .05), and Hispanic respondents also demonstrated significantly lower odds of PC knowledge (OR = 0.47; CI = 0.27, 0.83; p < .01), suggesting that patient- and community-facing educational campaigns are needed to improve awareness and reduce misperceptions of PC, particularly in rural and micropolitan areas.
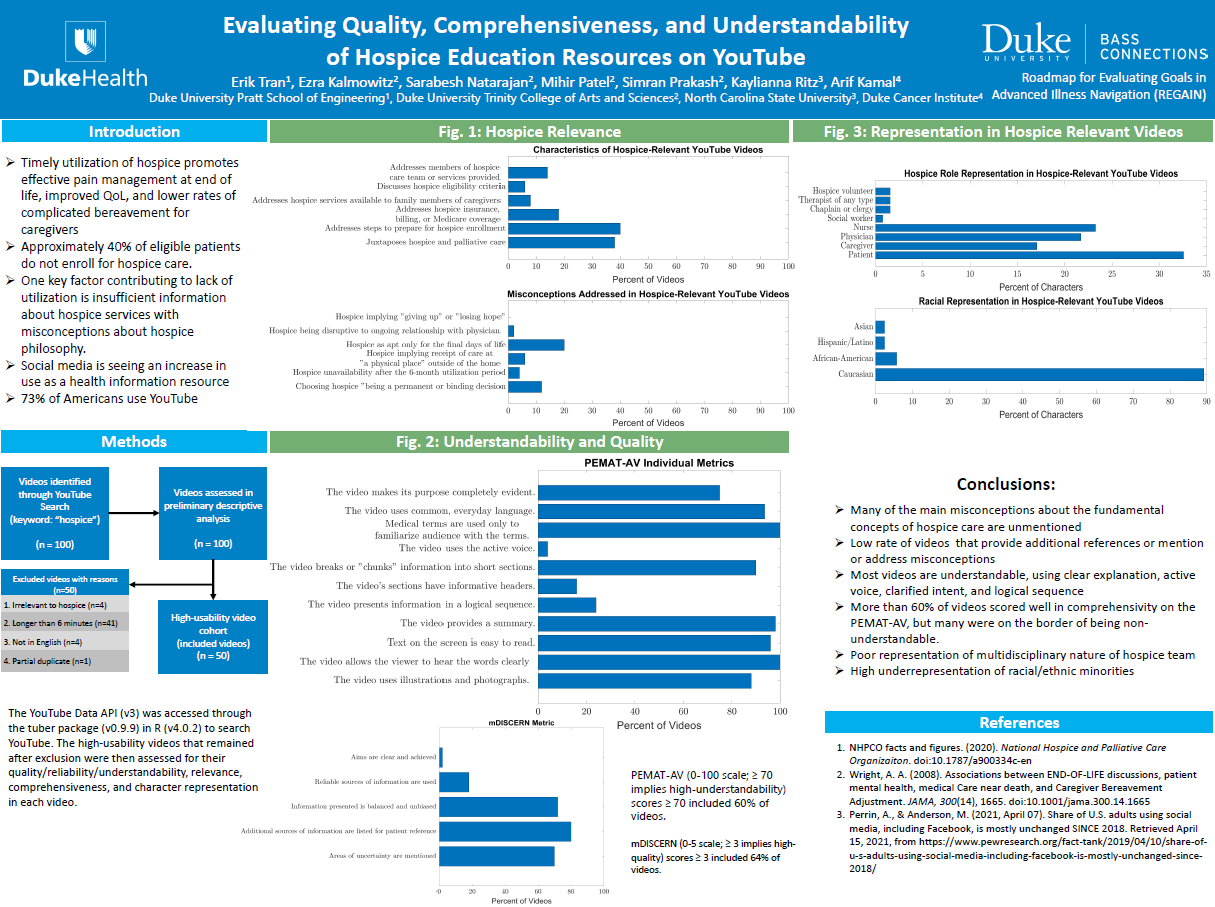
Evaluating Quality, Comprehensiveness and Understandability of Hospice Education Resources on YouTube
Poster by Erik Tran, Ezra Kalmowitz, Sarabesh Natarajan, Mihir Patel, Simran Prakash, Kaylianna Ritz and Arif Kamal
The poster summarizes my group's assessment of the quality of hospice education on YouTube by assessing relevance to hospice care, clarity in delivery, and quality of the information.