Impact of Face Covering on Patient Communication and Health Outcomes (2020-2021)
This project team evaluated the impact of mandatory face mask use by healthcare providers and patients on communication and health outcomes in the outpatient setting. Focusing on adults over the age of 60, team members developed a survey using novel and validated measures to assess how patients self-reported the ease of communication, listening effort, anxiety, ability to participate in social activities and health literacy.
Ultimately collecting data from 106 patients seen at Duke, the team utilized statistical analyses to determine if there were differences in self-reported outcome measures by hearing status and/or mask type. The team is currently in the process of submitting a manuscript and developing educational materials on communication strategies for broader healthcare communities.
Timing
Fall 2020 – Spring 2021
Team Outputs
Manuscript (in development)
Tips for Communicating with Patients While Wearing a Mask
This Team in the News
Two Faculty Receive Inaugural Bass Connections Leadership Award
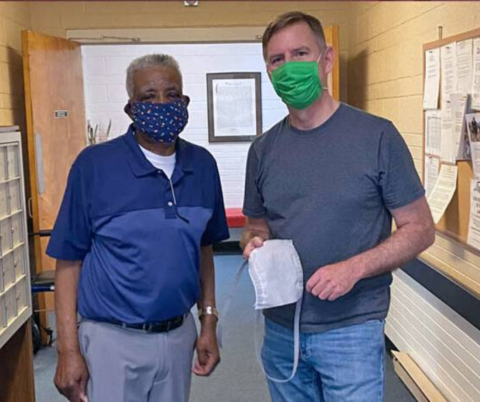
Image: Eric Westman, right, a physician at the Duke Outpatient Clinic and founder of Covering the Triangle, makes a delivery to Willie Patterson, staff member at a Crest Street neighborhood senior home, by Sam Miglarese/Duke Today
Team Leaders
- Howard Francis, School of Medicine-Head and Neck Surgery and Communication Sciences
- Juliessa Pavon, School of Medicine-Medicine: Geriatrics
- Kristal Riska, School of Medicine-Head and Neck Surgery and Communication Sciences
/graduate Team Members
-
Mikaela Matela, Cardiac Ultrasound
-
Hannah Wessler, Medicine-MD
-
Jessica West, Sociology-PHD, Sociology-AM
/undergraduate Team Members
-
Jiayin Bao, Music (AB)
-
Bhavika Garg, Neuroscience (BS)
-
Dana Guggenheim, Interdepartmental Major
-
Zella Hanson, English (AB)
-
Ila Kaul, Neuroscience (AB)
-
Margaret Lim, Biology (BS)
-
Kevin Wiafe, Psychology (BS)
/yfaculty/staff Team Members
-
Sherri Smith, School of Medicine-Head and Neck Surgery and Communication Sciences
-
Heather Whitson, School of Medicine-Medicine: Geriatrics
